The Centers for Disease Control and Prevention (CDC) just dropped a scary report about superbugs in the U.S. These germs, called “nightmare bacteria,” are getting way harder to kill. From 2019 to 2023, cases jumped big time. Doctors worry because our strongest meds don’t work on them anymore. This could mean more sick people in hospitals, especially the really ill ones. Don’t panic, but pay attention. Good habits like handwashing can help stop the spread. In this easy read, we’ll break down what these bugs are, why they’re rising, who’s at risk, and simple steps to stay safe. With antibiotic resistance killing millions worldwide, now’s the time to learn and act.
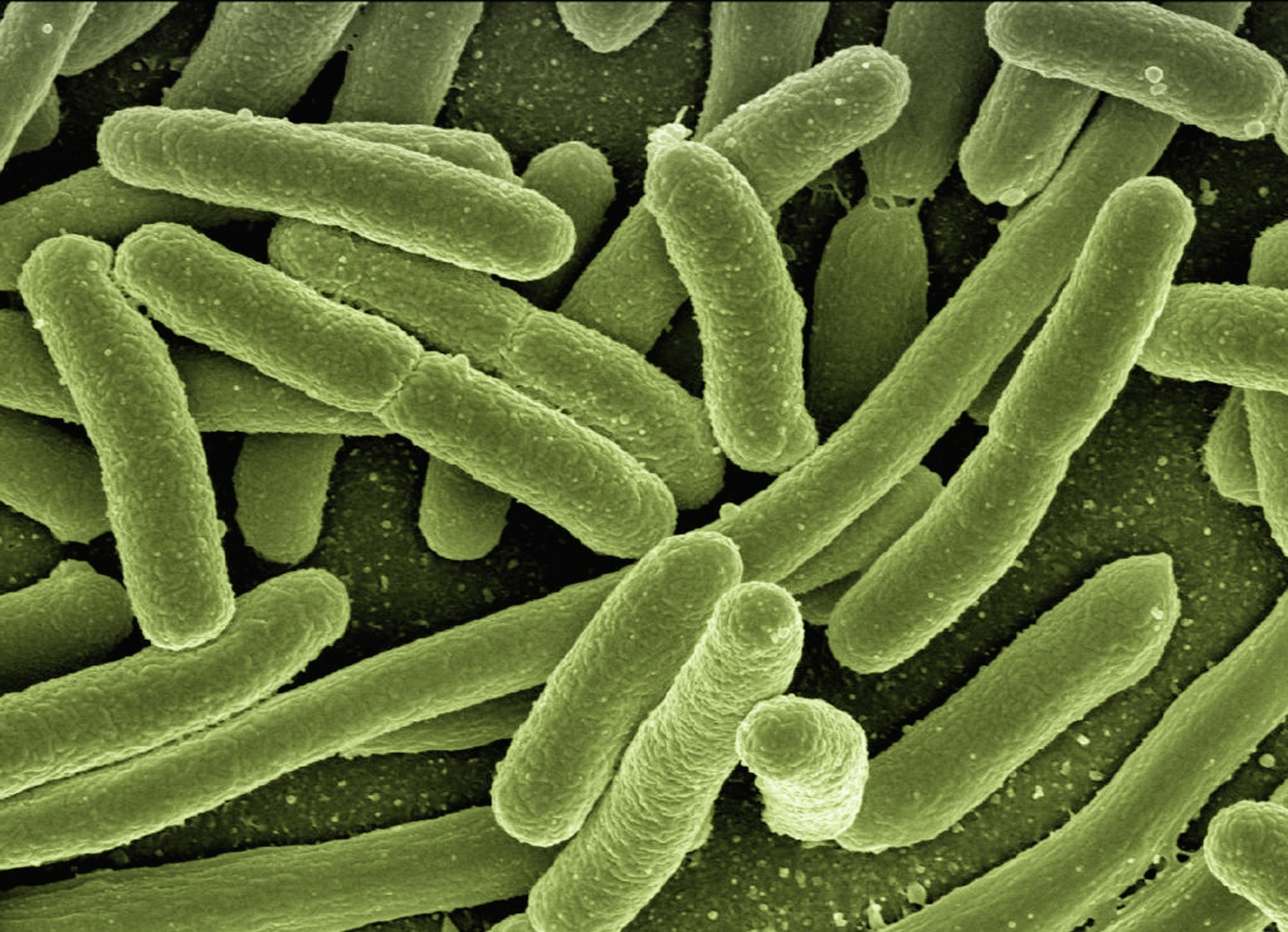
The report comes from the Annals of Internal Medicine. It tracks Carbapenem-resistant Enterobacterales, or CRE. These include common bugs like E. coli and Klebsiella pneumoniae. Normally, doctors use carbapenems—super-strong antibiotics—for bad infections. But CRE laughs them off. Inside CRE, there’s a worse group: Carbapenemase-producing CRE, or CP-CRE. These make an enzyme that chews up the drugs before they fight back. No meds left? That’s a nightmare for patients.
The big bad guy here is New Delhi metallo-β-lactamase CRE, or NDM-CRE. It’s tough against even new drugs made just for CRE. Between 2019 and 2023, CP-CRE cases rose 69% in 29 states—that’s over one-third of America. NDM-CRE? It shot up 461%! “This sharp rise is concerning,” said CDC expert Danielle A. Rankin, PhD. “It limits how we treat serious infections.” Back in 2020, CRE caused 12,700 infections and 1,100 deaths. Now, with the jump, experts fear worse.
Why the boom? Hospitals are ground zero. Sick folks get these bugs from shared tools or dirty hands. NDM-CRE spreads its “resist tricks” to other germs fast—like a bad rumor in a crowd. Healthy people? Low risk outside care spots. But if you’re in the hospital, watch out.
Who Gets Hit Hardest by These Superbugs?
Not everyone. These bugs pick on the weak. If you’re super healthy, you’re probably fine. But in hospitals, certain folks face big danger. Here’s who should be extra careful:
- Ventilator Users: Machines to help breathe can let bugs in through tubes.
- Device Dependents: Things like urinary catheters or IV lines are entry doors for germs.
- Antibiotic Takers: Long meds wipe good bugs, letting bad ones party.
- Weak Immune Systems: Cancer patients, elderly, or post-surgery folks can’t fight back easy.
Rankin notes: “This is among our sickest patients in healthcare.” No one-size-fits-all symptoms. It depends where it strikes. Urinary trouble? Pee pain or fever. Lungs? Cough and hard breaths like pneumonia. Blood? Chills and fast heart. Wounds? Red, oozy spots. Worst case: Brain swelling from meningitis. Spot it early—docs can pick the right (few) meds based on the bug type.
Treatment? Tricky. Almost no antibiotics work. “Limited options mean hard choices for docs,” said Marnie L. Peterson, PharmD, PhD from the University of Minnesota. She wasn’t on the report but knows the field. Tailor meds to your body—kidney issues or allergies make it tougher. Early tests save lives.
How Do These Nightmare Bugs Spread?
Contact is king. Touch an infected person, dirty table, or used tool—bam, you’re carrying it. You might not feel sick but pass it on (that’s colonization). Rare animal jumps happen too. In hospitals, it’s like a chain: One patient to nurse’s hands to next bed.
Stop it with basics. Wash hands a ton—soap for 20 seconds. Clean rooms and gear deep. Track cases to catch outbreaks fast. Peterson pushes: “Healthy folks help too, especially caregivers for old or sick loved ones.” If visiting grandma, scrub up!
This ties to the big “silent pandemic”: Antimicrobial resistance (AMR). Bugs beat drugs meant to zap them. Not just bacteria—viruses, fungi too. Common ones: MRSA skin boils, tough pneumonia from Streptococcus. C. diff? It loves gut chaos after antibiotics.
U.S. sees 3 million AMR infections yearly. Global deaths? Nearly 5 million in 2019. By 2050, The Lancet warns 39 million could die, with 1.91 million in one year alone—70% up from now. Scary stats, right?
Fighting Back: Stewardship and Smart Habits
Good news? We can fight. CDC and World Health Organization push “antibiotic stewardship.” It’s teams of docs, nurses, and experts cutting overuse. Better tests spot bugs quick. Research grows. “Progress exploded in five years,” Peterson said. Fewer wrong prescriptions mean slower resistance.
What can you do? Ask questions. Need that antibiotic for a cold? Probably not—save it for real bacterial fights. Finish full courses if prescribed. Farmers: Cut farm antibiotics too. Governments fund new drugs. But we need more—old ones lose power.
Hospitals lead with rules: Gown up for visits, no flowers in rooms sometimes. Public? Stay healthy—eat well, move, vaccinate. It cuts hospital trips.
The CDC report screams urgency. With NDM-CRE exploding, 2023 numbers dwarf 2019. States like California and New York see most cases. But all 50 could soon. “We face a growing threat,” Rankin warned.
Hope lies in action. Early catch, clean hands, wise meds. One study shows stewardship drops resistance 20% in hospitals. Global pacts like WHO’s aim for 10 million saved by 2030.
A Wake-Up Call for All
This isn’t sci-fi—it’s now. Nightmare bacteria turn simple infections deadly. But knowledge is power. Talk to your doc about resistance. Support clean policies. As cases climb, remember: Small steps stop big spreads.
The CDC’s warning? A lifeline. Heed it, and we beat the bugs. Stay informed, stay clean, stay safe. America’s health hangs in the balance—but together, we win.